Treatment options can seem overwhelming to people with inflammatory autoimmune diseases such as rheumatoid arthritis. An endless mixture of pain medications to disease-modifying antirheumatic drugs (DMARDs), immunosuppressants, NSAIDs, and an ever-growing list of biologic drugs. As a patient, the range of pharmaceuticals available leaves you confused about your choices but healthcare professionals are always available to give you medical advice. Today we will look at two drugs Xeljanz and Humira and how they compare to one another. Read on to find out more.
What is Humira?
Humira is an immunosuppressant medication manufactured by Abbvie Pharmaceuticals. It is classed as a tumor necrosis factor (TNF) inhibitor or an anti-TNF, containing the active ingredient adalimumab.
Humira is approved by the FDA to treat the following inflammatory autoimmune diseases:
- Rheumatoid arthritis in adults
- Active psoriatic arthritis in adults
- Ankylosing spondylitis in adults
- Moderate to severe plaque psoriasis in patients who are candidates for systemic therapy or phototherapy in adults
- Juvenile idiopathic arthritis in children aged 2 years and older
Humira is also approved to treat similar non-autoimmune inflammatory diseases:
- Crohn’s Disease in adults and children aged 6 years and older
- Ulcerative colitis in adults and children aged two years and older
- Hidradenitis suppurativa in adults and children aged 12 years and older
How does Humira work?
Humira works specifically as a TNF blocker, to treat inflammation. TNF alpha (tumor necrosis factor-alpha) is one of a number of different antibodies produced by white blood cells and other parts of the immune system.
Once Humira is injected into your body, its active ingredient helps reduce inflammation. Your immune system releases a protein in your body to trigger inflammation called TNF-alpha (tumor necrosis factor-alpha). The active ingredient in Humira attaches to TNF-alpha preventing it from working. This limits the amount of inflammation your immune system can cause.
By reducing inflammation, Humira can provide relief from the symptoms of inflammatory diseases. It can also limit the damage caused and stop flare-ups from happening.
What is Xeljanz?
Xeljanz is a prescription medication and the first drug in its class of Janus Kinase Inhibitor (JAK) drugs. It is given to adults to treat the following inflammatory autoimmune diseases:
- Moderate to severe active rheumatoid arthritis in adults who have previously not responded well to a medication called methotrexate
- Moderate to severe psoriatic arthritis in adults who have previously not responded well to a medication called methotrexate or to other disease-modifying antirheumatic drugs
- Moderate to severe ulcerative colitis in adults who have previously not responded well to TNF blocker medications
How does Xeljanz work?
The active ingredient in Xeljanz is called tofacitinib, classed as a JAK inhibitor drug. It reduces the amount of inflammation in your body. Tofacitinib works by blocking the action of two enzymes in your body called Janus Kinase 1 (JAK1) and Janus Kinase 3 (JAK 3). These two enzymes are used by your immune system to trigger inflammation. By blocking these enzymes, tofacitinib reduces how much inflammation your immune system can cause.
How do you take Xeljanz and Humira?
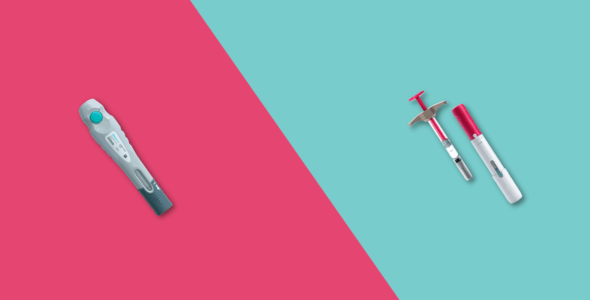
You take Humira by subcutaneous injection (injecting it under your skin) using either a pre-filled syringe or an injectable pen. It is important to use a new needle each time to prevent the risk of infection. You may have injection site reactions such as redness, bruising, or irritation after administration that will settle down after a few hours. Humira can be given at home through an injection. You will be trained on how to self-administer the injection or it could be done with help from a family member or friend.
Xeljanz on the other hand is taken by mouth with or without food and comes in two forms. The two forms are Xeljanz immediate-release and Xeljanz XR extended-release.
What are the side effects of Xeljanz and Humira?
The most common side effects caused by both Xeljanz and Humira include:
- Headaches
- Upper respiratory tract infections
- Rashes
With Xeljanz:
- Diarrhea
- Increased cholesterol levels
With Humira:
- Injection site reactions
- Stomach pain
Occasionally, Xeljanz and Humira can cause more serious side effects:
- Severe allergic reactions to the medication
- An increased risk of serious infections e.g herpes zoster
- An increased risk of developing certain cancers, including lymphoma and other skin cancers
- High blood pressure (hypertension)
- A risk of death in patients with rheumatoid arthritis who are over 50 and who have at least one heart disease risk factor
Is Xeljanz more effective than Humira?
A head-to-head study called the Oral Rheumatoid Arthritis triaL (ORAL) has been carried out between the two drugs. It was led by Professor Roy Fleischmann a leading Rheumatologist and the results were published in The Lancet.
It was a 12 month, double-blind head to head study with over 1000 patients put into three groups
- Xeljanz 5mg twice a day (monotherapy)
- Xeljanz 5mg twice a day with a weekly dose of methotrexate
- Humira 40mg every 2 weeks via subcutaneous injection with a weekly dose of methotrexate
In this clinical trial, each patient’s response to treatment was measured using the American College of Rheumatology’s (ACR) scoring system. Having a score of ACR50 was the primary endpoint in the study meaning that the person had a 50% reduction in their rheumatoid arthritis symptoms. At 6 months, ACR50 was achieved in 46% of patients with Xeljanz and methotrexate, and 44% of patients with Humira and methotrexate. The tofacitinib monotherapy group achieved ACR50 in 38% of patients.
We can say both Xeljanz and Humira were similarly effective in reducing disease activity. The choice of treatment of rheumatoid arthritis, therefore, depends on individual factors such as the severity of disease and medical history which can be discussed with your healthcare professional.
What are the alternatives to Xeljanz and Humira?
As mentioned earlier there are many treatments available here are a few alternatives to look at: Simponi (golimumab), Remicade (infliximab), Rituxan (rituximab), Enbrel (etanercept), and Orencia (abatacept).
Should I avoid certain vaccines during Xeljanz and Humira treatment?
Yes. If you are taking Xeljanz or Humira you are advised to avoid live vaccines because they can put you more at risk of infection. Xeljanz and Humira dampen down your immune system, making you more prone to infection.