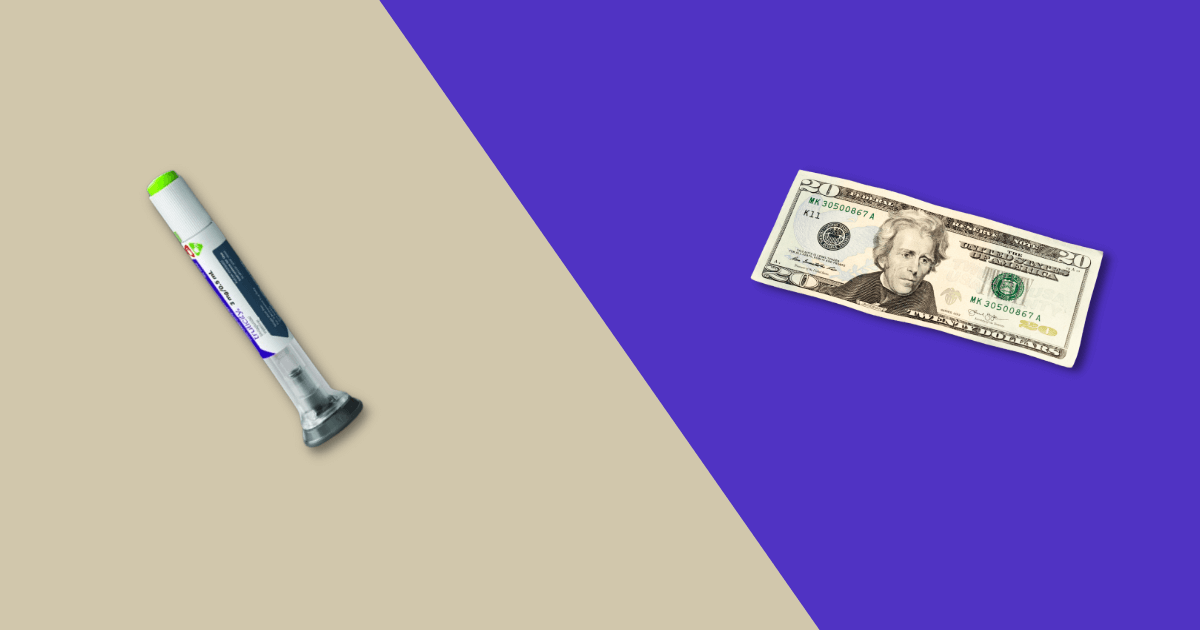
Wegovy injection (semaglutide) is an FDA-approved injectable GLP-1 medication approved for chronic weight management in adults who are overweight or have obesity. As the #1 prescribed medication for chronic weight loss in the United States, there is high demand for this medication due to its proven effectiveness, resulting in a shortage in the supply.
For those seeking an easy and hassle-free method to obtain Wegovy online, getting a prescription or filling it out online at home is possible. This guide outlines the necessary steps to purchase Wegovy conveniently from your home.
Step 1: Speak with an online healthcare provider
Start by scheduling an online consultation with a certified healthcare provider who specializes in weight management and can issue the prescription if medically appropriate, as Wegovy is a prescription medication. The healthcare provider can assess your eligibility for a prescription and discuss whether the medication is suitable for your weight control goals and health needs.
If you don’t have a regular healthcare provider, you can easily book one through a telehealth service such as the NiceRx medical weight loss program. These services offer quick appointment scheduling, often within 48 hours, making it convenient to connect with a licensed clinician who can prescribe Wegovy or compounded semaglutide (same active ingredient as Wegovy) for weight management.
Step 2: Meet with the healthcare provider online
To proceed with getting Wegovy online, the next step involves meeting with a certified healthcare provider via online consultation. During this consultation, you can discuss your weight loss goals and medical history with your provider. They will assess your health status and check whether you meet the criteria for Wegovy treatment.
Your provider may ask for certain details concerning your medical history before prescribing Wegovy to ensure that you are in good health and do not have any underlying conditions that could pose risks while taking Wegovy.
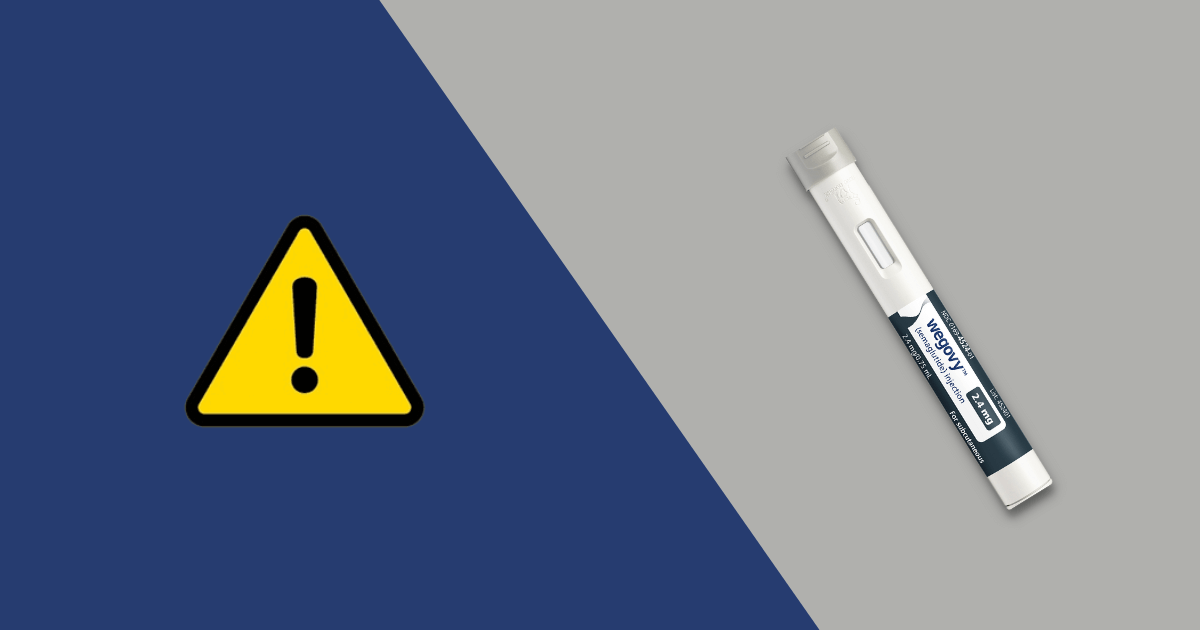
It’s essential to discuss the potential risks and side effects of Wegovy with your provider during the consultation. The most common side effects with an incidence of 5% or higher include abdominal pain, headache, nausea, vomiting, dyspepsia, etc. Anti-nausea medication is often prescribed alongside this medication. There are some serious adverse effects associated with Wegovy, such as pancreatitis, serious allergic reactions, increased heart rate, etc. Your doctor will help assess whether the benefits of Wegovy outweigh its potential risks for your health profile. You should seek immediate medical advice from your provider if you experience any adverse side effects.
Step 3: Get a Wegovy prescription for weight loss
The third step involves receiving a prescription from your provider. The provider will issue a prescription only if you are eligible to receive this medication based on your health history to ensure that it is safe to take the medication as prescribed. This medication should be used alongside a reduced calorie diet and increased physical activity.
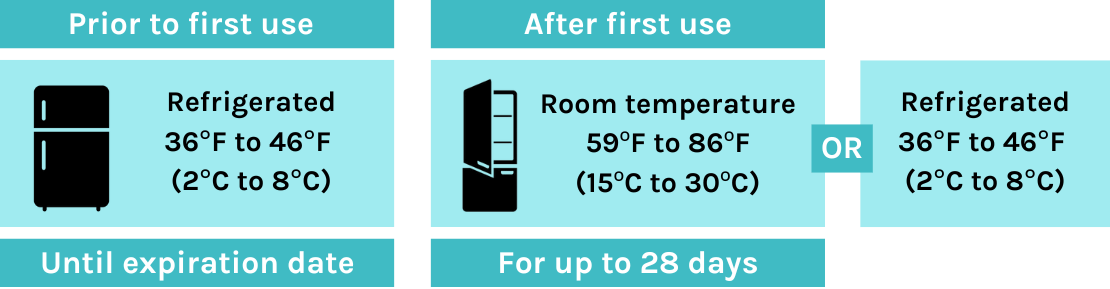
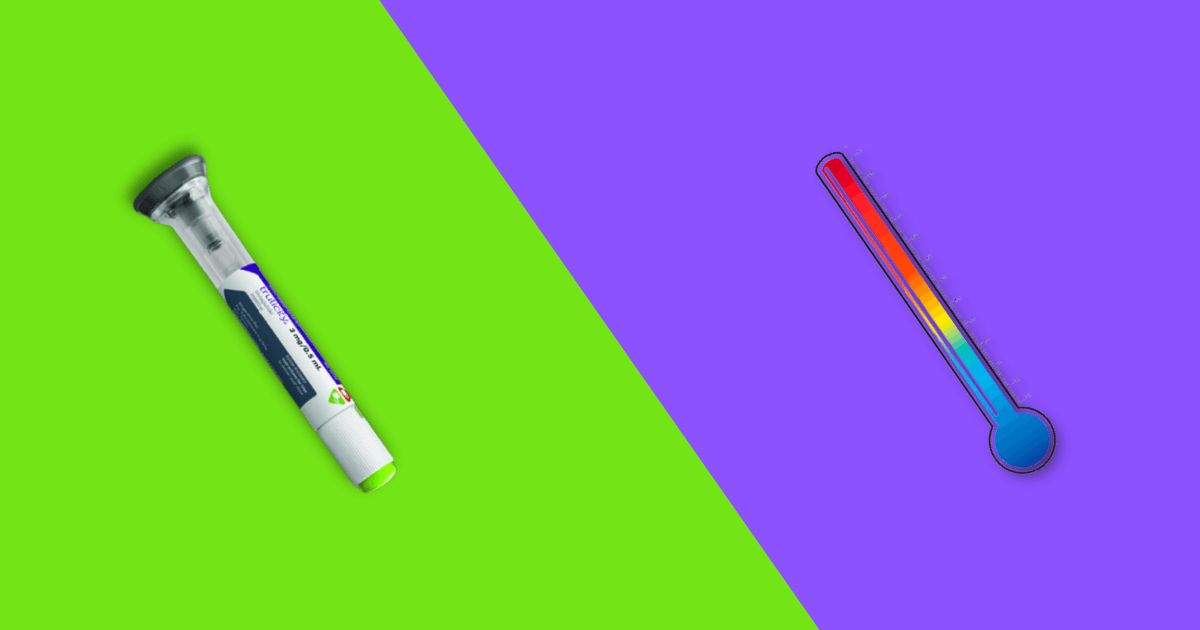
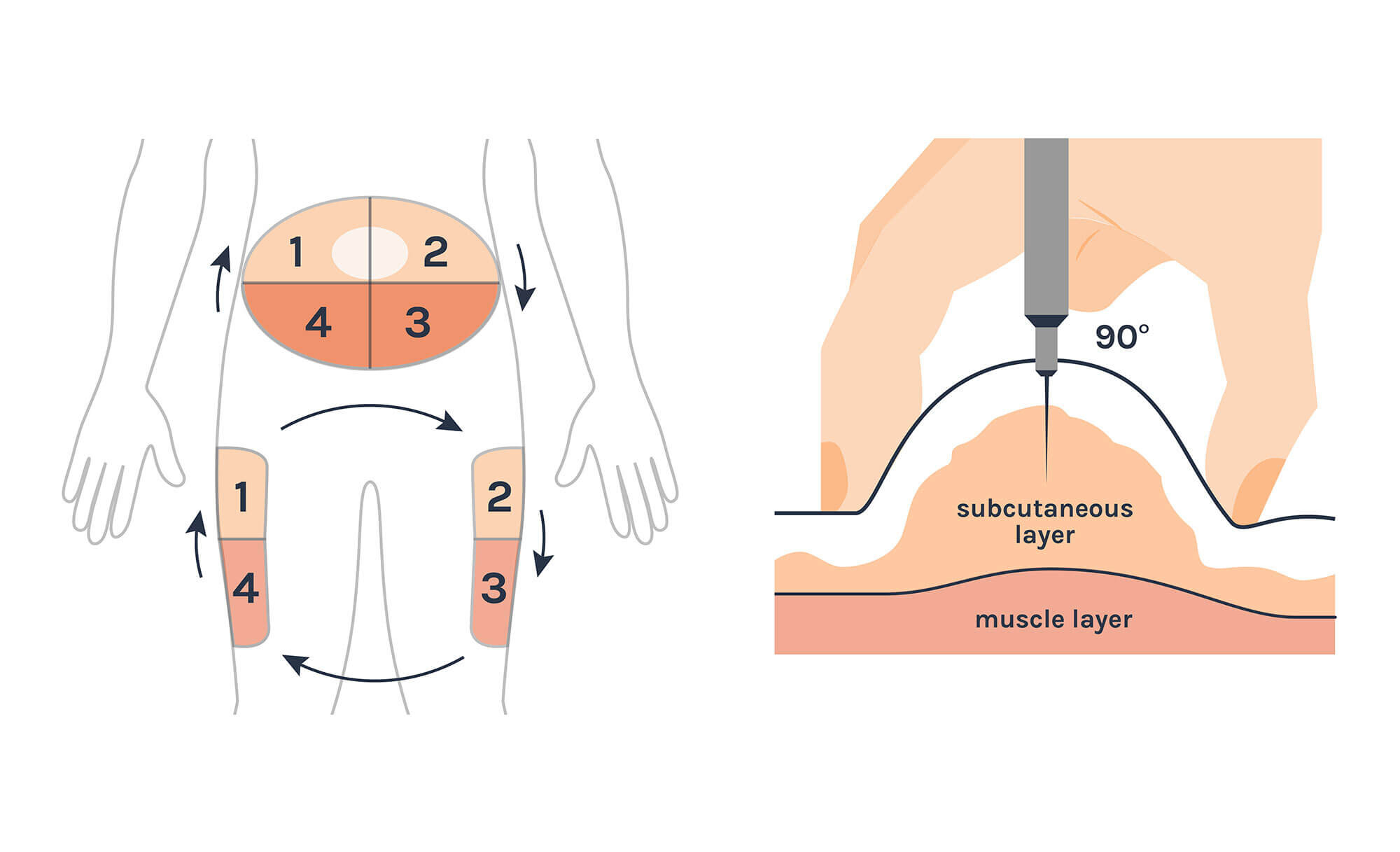
Wegovy is available in 5 different strengths. Your provider will prescribe a low dose of Wegovy initially with 0.25 mg then escalate to the maintenance dose of 0.5 mg, 1 mg, 1.7 mg, or up to 2.4 mg. They will prescribe injections delivered through pre-filled syringes or single-dose pens to administer the doses based on your convenience.
Along with the prescription, your provider will explain how to administer the medication, what to do when you skip a dose, and possible side effects associated with the medication. Follow-up visits may be necessary to obtain new prescriptions as your dosage increases. These appointments allow your provider to optimize your treatment plan, ensuring you receive the maximum benefit from Wegovy while addressing any concerns or adjustments needed along the way.
Step 4: Get prior authorization from your insurance if needed
The fourth step in obtaining Wegovy is ensuring you have prior authorization from your insurance provider. Be sure to check with your insurance provider to see if you need prior authorization for Wegovy to be covered under insurance. Your healthcare provider’s office can assist you in obtaining this authorization by submitting the necessary documentation, including medical necessity and supporting clinical information for insurance coverage.
By obtaining prior authorization, you can smoothly integrate Wegovy into your weight loss journey while ensuring financial coverage for your treatment.
Step 5: Navigate challenges with Wegovy shortages
Novo Nordisk is putting lots of effort into increasing Wegovy production, now seeing 25,000 new U.S. patients start weekly. Despite this, demand still exceeds supply.
To manage your Wegovy prescription, contact your pharmacy well in advance for refills and be specific about your dose. If shortages persist, consult your healthcare provider about where to find Wegovy in stock or for alternative solutions.
Novo Nordisk has committed to resolving issues, operating manufacturing lines around the clock, and making significant investments in new facilities.
You can check the FDA report for Wegovy dose availability and shortage reasons.
Step 6: Buy Wegovy online or at a local pharmacy
The final step to getting Wegovy online is ensuring your prescription is filled by a reputable online pharmacy.
According to U.S. law, you can buy Wegovy online under the Federal Food, Drug, and Cosmetic Act only with a valid prescription. This prescription must be for a genuine medical need and must be issued by a medical professional that is licensed in your state.
Once you have had an online consultation with a certified medical professional and checked the coverage status, you can proceed to purchase the medication online.
There are many national pharmacies and local pharmacies that offer home delivery services. Check if the pharmacy provides this option for your added convenience. Additionally, it’s important to verify that the pharmacy has adequate stock of Wegovy before placing your order.
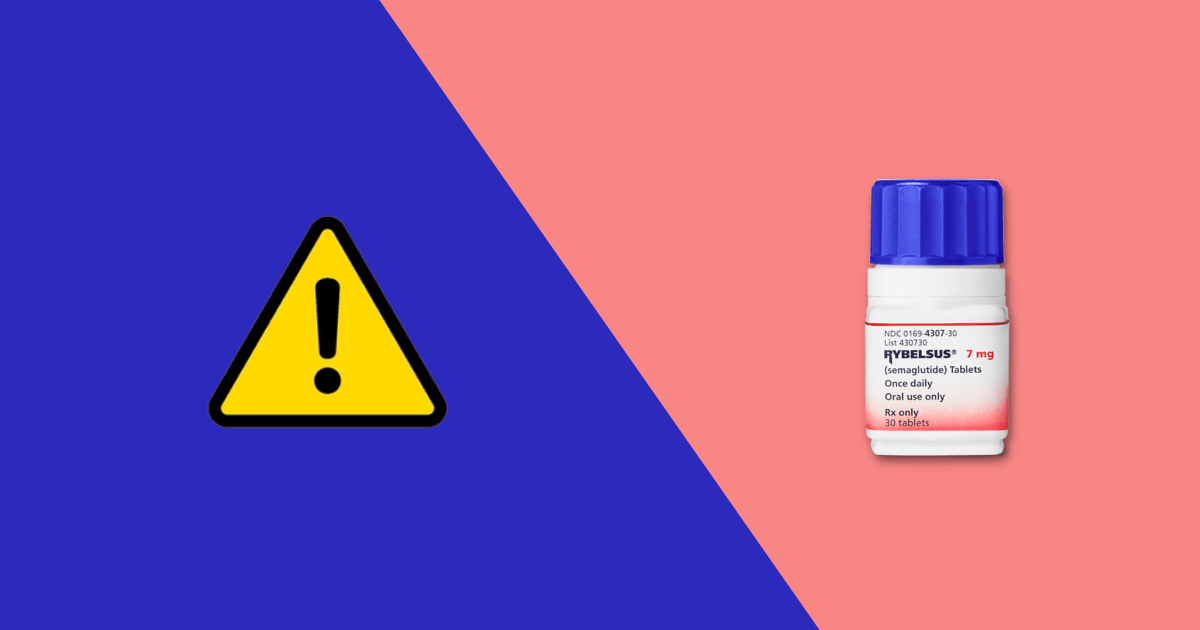
If Wegovy shortages persist, compounded semaglutide might be an alternative available from compounding pharmacies. However, FDA advises against using a compounded drug if it contains salt. If considering compounded semaglutide, consult your healthcare professional to discuss potential risks and benefits.
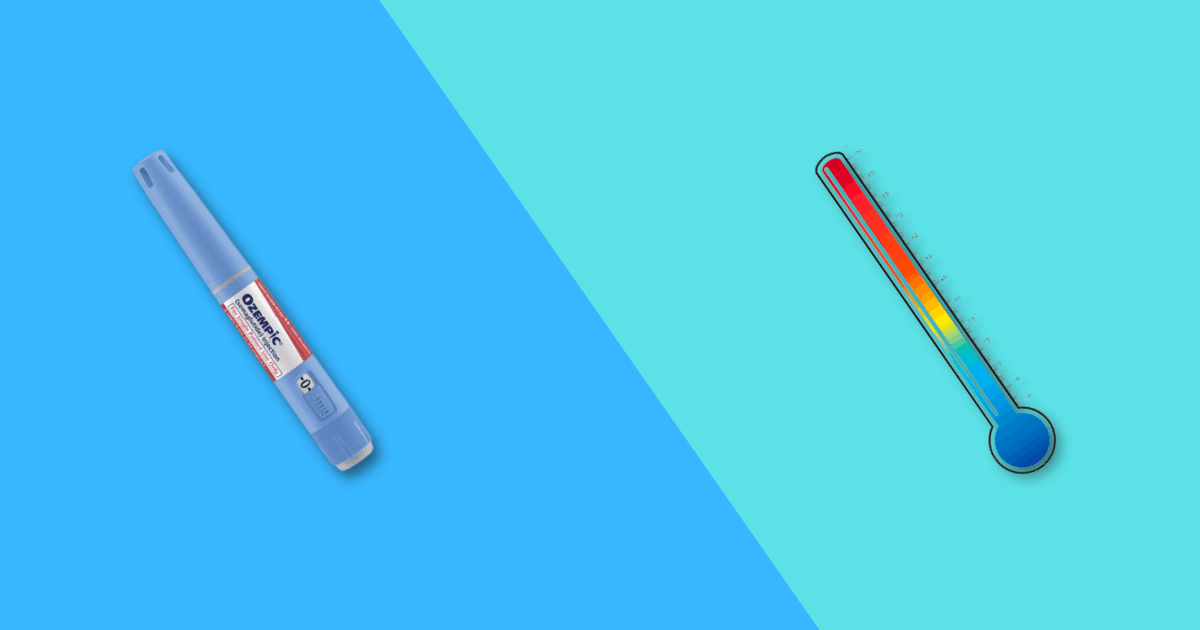
Some individuals might consider Ozempic as an alternative to Wegovy since both medications contain the active ingredient semaglutide. However, manufacturers advise against this interchangeability due to FDA approvals for distinct indications. Ozempic is approved for managing type 2 diabetes, while Wegovy is specifically approved for chronic weight control. Nonetheless, Ozempic is commonly prescribed off-label.
Speak with an online provider through NiceRx
You can contact an online provider at NiceRx. At NiceRx, our team of experts are dedicated to providing guidance and support for purchasing medications online, including compounded Semaglutide which contains the same active ingredient as Wegovy. Our telehealth services allow you to consult with healthcare professionals who can assist you throughout the process.
FAQs about getting Wegovy online
Is it legal to buy Wegovy online?
Yes, it is legal to buy Wegovy online, provided that the purchase is made with a valid prescription from a certified provider, issued for a legitimate medical purpose. According to US law, this prescription must be based on a medical evaluation of the patient by the prescribing practitioner or a covering practitioner.
Do you need a prescription for Wegovy?
Yes, you need a valid prescription to buy Wegovy, whether from a local pharmacy or online. Wegovy is a prescription-only drug, and the prescription must be issued by a valid medical professional in your state.
How do I get an online prescription for Wegovy for weight loss?
To obtain an online prescription for Wegovy for weight loss, start by scheduling an appointment with a certified physician who offers telehealth services. During your online consultation, discuss your weight loss goals and provide your medical history including any other prescription and over-the-counter medicines, vitamins, and herbal supplements you are currently taking to the physician. They will assess your eligibility criteria for Wegovy based on medical guidelines and evaluate whether it is suitable for your health condition. If the physician determines that Wegovy is appropriate for you, they will issue a prescription.
What are the requirements to qualify for a Wegovy prescription?
To qualify for a Wegovy prescription, adults must have obesity or be overweight with a body mass index (BMI) of 30 kg/m² or greater, or 27 kg/m² or greater with at least one associated weight related health condition such as high blood pressure, type 2 diabetes mellitus, or abnormal cholesterol levels. Additionally, adolescents aged 12 and above must have an initial BMI at the 95th percentile or greater for their age and sex. Both adults and adolescents should also be following a reduced-calorie diet and engaging in increased physical activity as part of their weight control efforts. These criteria ensure that Wegovy is prescribed appropriately to support effective weight loss and improve overall health outcomes.
What about Wegovy for people with heart disease?
On March 2024, Wegovy was approved for helping to reduce the risk of heart attack, stroke, and cardiovascular death in people with heart disease and overweight or obesity. This medication will help with your overall cardiovascular health.
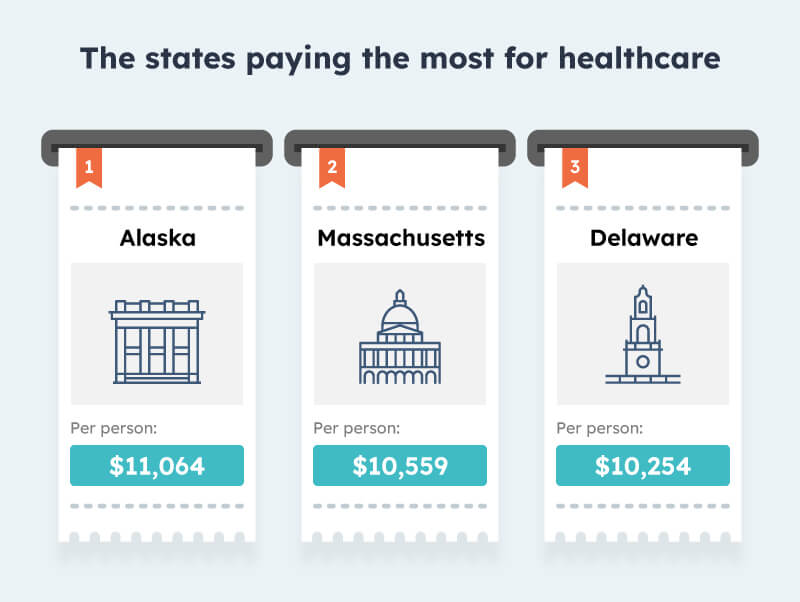
How much does Wegovy cost?
The cost of wegovy can vary depending on factors such as insurance coverage, pharmacy pricing, and eligibility for savings programs. Without insurance, the list price for a one-month supply of Wegovy is approximately $1,349.02. However, many patients may pay significantly less through insurance plans or savings offers. You can check about insurance companies that provide insurance coverage and savings offers online.
Who should not use Wegovy?
Wegovy should not be used by individuals with certain medical conditions or risk factors. Specifically, do not use this weight loss drug if:
- You or your family had a health condition related to the thyroid or endocrine system like medullary thyroid carcinoma and Multiple Endocrine Neoplasia syndrome type 2.
- You have had a serious allergic reaction like swelling of your face, lips, tongue, or throat; fainting or feeling dizzy; problems breathing or swallowing to semaglutide or any of the ingredients in Wegovy.
- You are pregnant or planning to become pregnant, as Wegovy may cause fetal harm. When pregnancy is recognized, discontinue the medication immediately.
- For females and males of reproductive potential, discontinue Wegovy at least 2 months before a planned pregnancy due to the long half-life of semaglutide.
Will I lose weight with Wegovy?
Yes, you will start losing weight after taking Wegovy as it is an approved and potent weight loss medication. It has been shown to help individuals lose a significant amount of weight when used in conjunction with a reduced-calorie diet and increased physical activity. You can check your potential weight loss with Wegovy. Studies have demonstrated that semaglutide, the active ingredient in Wegovy, leads to significant weight loss, ranging from 9.6% to 17.4% of initial body weight. However, a new medication, tirzepatide, marketed under the brand name Mounjaro, has shown even greater efficacy, with clinical trials reporting weight loss of up to 20.9% of initial body weight.
What happens after I stop taking Wegovy?
After you stop taking Wegovy, you may regain weight. A study found that one year after stopping Wegovy and lifestyle changes, people regained about two-thirds of the weight they had lost, and their cardiometabolic health, such as blood pressure and cholesterol levels, also worsened.